Historically in the U.S., health improvement for individuals has been focused around doctor’s offices and the healthcare system. While this has been the emphasis, healthcare costs have risen exponentially while health outcomes have only improved slightly. As a result, we have seen a shift in the focus from having doctors improve health to a more holistic approach that encompasses what the industry calls Social Determinates of Health (SDH).
While you may have been hearing that phrase, Social Determinates of Health buzzing around, more than likely you have asked yourself, what does that even mean? At the very basic level, SDH are factors that influence a person’s health like income, education, the neighborhood and physical environment that they live in, employment, social support networks like friends and family, and their access to healthcare services including doctors, dentists, hospitals, and specialists. When you look at health through this lens you see that every aspect of a person’s life impacts their wellbeing. The flip side is also true. If a doctor only sees what a person presents in the exam room and doesn’t ask about or address all the other influencing elements, the doctor will more than likely be unsuccessful in fully treating a person.
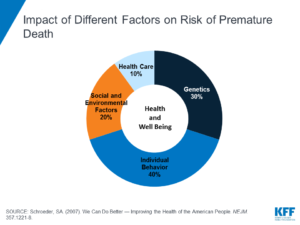 Healthcare services only make-up 10% of the puzzle when it comes to someone’s health and wellness. A person’s behaviors–like diet, exercise, tobacco use–have the most impact on a person’s health at 40%. Genetics make up about 30% of someone’s health status and SDH make up 20% of a person’s health. As we are becoming more and more aware of how SDH influence health, TCHNetwork and our partners are working to address them both within the healthcare sector and out.
Healthcare services only make-up 10% of the puzzle when it comes to someone’s health and wellness. A person’s behaviors–like diet, exercise, tobacco use–have the most impact on a person’s health at 40%. Genetics make up about 30% of someone’s health status and SDH make up 20% of a person’s health. As we are becoming more and more aware of how SDH influence health, TCHNetwork and our partners are working to address them both within the healthcare sector and out.
One way SDH have been incorporated into healthcare is through screening patients at primary care clinics, emergency rooms, and other points of contact with the healthcare system. Screening tools ask questions about access to housing and food, interpersonal violence, transportation needs, and demographic information such as income level, gender identity, race/ethnicity, and age. These screenings give providers an extra tool in their tool belt when it comes to treating the whole health of their patients and allows for the doctor’s office to connect patients to resources like food banks, free transportation options, and nonprofit organizations that can help address a person’s SDH needs.
TCHNetwork is currently in year two of a five-year project meant to address the gaps between clinical care and community services around SDH. The project, Accountable Health Communities Model (AHCM), is a federally funded pilot program with 22 sites around the country working to implement a validated screening tool into healthcare settings. The Center for Medicare and Medicaid Services, the agency supporting the pilot, will collect data on the results of the SDH screening tool and use that data to look at ways we can modify our system to better address the needs of our communities across the nation.
TCHNetwork is the Community Lead Organization on the AHCM working with numerous other organizations across Colorado’s Western Slope including Rocky Mountain Health Plans. Our role, among many things, is to recruit practices in San Miguel, Ouray, Montrose, Delta and Gunnison counties to use the SDH screening tool at their practice. We are excited at the prospect of better understanding the social needs of our communities and connecting people with the resources they need to lead a happier and healthier life.
Hopefully, the next time you visit your doctor you will find yourself answering questions about the social factors that determine your health and wellness—and knowing why this information is so important for your doctors to know!
–Adrienne Christy, Community Health Programs Manager
If you represent a practice and are interested in learning more about becoming a screening site, please contact Adrienne at CHPM@tchnetwork.org